NIH-funded study in a small group of individuals shows preliminary results that could lead to new pain treatments.
In a recently published study, researchers have for the first time measured pain-related brain activity in real time from inside the brains of people with chronic pain disorders due to stroke or amputation (phantom limb pain). Recording signals were collected over months while patients were at home. The data were then analyzed with machine learning tools to identify patient-specific chronic pain signatures. These findings, published in Nature Neuroscience, were funded by both the National Institutes of Health’s Brain Research Through Advancing Innovative Neurotechnologies® (BRAIN) Initiative and the Helping to End Addiction Long-term® Initiative, or NIH HEAL Initiative®, represent a first step towards developing novel methods for tracking and treating chronic pain.
What is chronic pain? Chronic pain is a significant contributor to disability worldwide and a major contributor to the nation’s opioid crisis. Although neuropathic pain is caused by damage to nerves, chronic neuropathic pain is a brain disorder. It does not respond well to current treatments and can be debilitating for people living with the conditions.
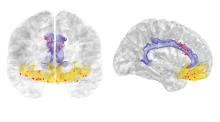
What does this study show? Four participants, three with post-stroke pain and one with phantom limb pain, were surgically implanted with electrodes targeting their anterior cingulate cortex (ACC) and the orbitofrontal cortex (OFC). These two regions in the brain are involved in the perception and emotional response to chronic pain, respectively. Scientists measured patient-specific pain signals in these regions and found that chronic pain signatures can track individual pain episodes in real-time – offering the potential for personalized therapies such as targeted brain stimulation.
Why is this research important? This study represents an initial step toward uncovering the patterns of brain activity that underly chronic pain. Individual pain signatures that can predict pain accurately will be useful for both patient-specific treatments and new types of therapies. The most immediate benefit may be to inform ongoing studies in both HEAL and BRAIN research to use deep brain stimulation (DBS) as a novel way to treat chronic pain.
Effective and non-addictive treatments for chronic pain conditions is a main goal of HEAL efforts to find scientific solutions to stem the opioid public health crisis. The development of new technologies and advances to better understand brain circuits is a key aim of the NIH BRAIN Initiative. The findings are a key step to identifying pain-specific biomarkers toward personalizing pain management for individuals.
This study was funded by the NIH BRAIN Initiative (UH3NS109556), NIH HEAL Initiative (UH3NS115631) and Defense Advanced Research Projects Agency (DARPA).
To read more about this study, visit the press release or explore the findings in Nature Neuroscience.
Image credit: Prasad Shirvalkar, M.D., Ph.D., UCSF
